Nerves are specialized tissues that carry signals to and from the brain to different body regions. These signals help you feel sensations like touch, pressure, pain, and temperature. They are also involved in your movement and control of certain body functions such as heartbeat and digestion.
What is Diabetic Neuropathy?
The medical term ‘neuropathy’ means nerve damage. Diabetic neuropathy is nerve damage that occurs in individuals with Diabetes. In diabetes, high sugar (glucose) levels can result in nerve damage in various parts of the body. Most often, the nerves in the hands and in the feet are affected (peripheral neuropathy). According to research studies, diabetic neuropathy develops in as many as 50% of people with diabetes during their lifetime. Neuropathy can affect those with type 1 and type 2 diabetes.
What are the symptoms of Diabetic Neuropathy?
Four main types of neuropathy are seen in individuals with diabetes. The symptoms depend on the type of neuropathy and the nerves involved. A person can develop one or more than one type of neuropathy. In the initial stages, no symptoms may be noted. Symptoms develop slowly when significant nerve damage has happened.
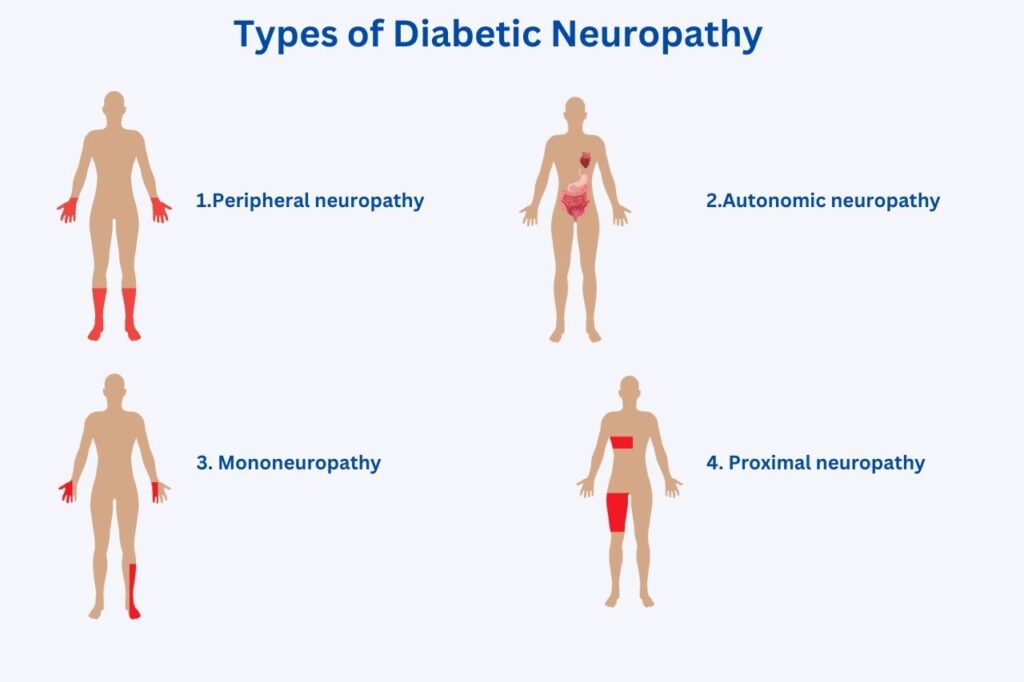
1. Peripheral neuropathy
This is the most common type of diabetic neuropathy. In this condition, nerve damage is seen in the limbs. The feet and legs are more often affected than the arms and legs. It is also known as distal symmetric polyneuropathy (DSPN). Symptoms of peripheral neuropathy can include:
- Decreased ability to feel touch, pain, hot, and cold sensations
- Tingling or burning sensation in the limbs
- Increased sensitivity to touch (even light objects touching limbs may feel painful)
- Aches or cramps
- Muscle weakness
- Ulcers, infections and damage to bone and joints (in severe cases)
2. Autonomic neuropathy
Autonomic nerves control the functions of internal organs of the body such as the heart, digestive system, eyes, urinary bladder, sex organs, and sweat glands.
When diabetes affect nerves in these organs, you may experience certain symptoms that include:
- Increased heart rate (even at rest)
- Feeling dizzy or fainting when standing from sitting or lying down position due to sudden drop in blood pressure (orthostatic hypotension)
- Urinary problems such as difficulty to pass urine (urinary retention), inability to control urine (urinary incontinence), and frequent infections in the urinary tract.
- Digestive problems such as difficulty swallowing, feeling of fullness, nausea, and vomiting due to slowness of digestive system
- Constipation (reduced motions) or diarrhoea (increased motions) or a combination of both
- Men can have problems getting proper erections
- Women can experience dryness in the vagina and other sexual problems
- Feeling more warm or cold (temperature control problems)
- Excessive sweating or reduced sweating
- Difficulty in adjusting the vision when looking at nearby objects after looking far or when shifting from light to dark.
- Decreased awareness of symptoms of low blood sugar (hypoglycemia unawareness)
3. Mononeuropathy (Focal neuropathy)
Mononeuropathy is a condition where there is damage to a single nerve, most commonly in the arm, leg, head or torso. Mononeuropathy can appear suddenly and subside by itself within a few weeks or months.
The symptoms depend on the specific nerve that is involved and may include:
- Paralysis on one side of the face
- Difficulty in focussing the eyes, or double vision
- Pain in the foot or shin
- Pain in the front part of the thigh
- Numbness or tingling in the hand or fingers, and weakness of hand-grip causing dropping of objects from hands (Carpal tunnel syndrome)
4. Proximal neuropathy (Diabetic radiculopathy)
This is a rare but disabling form of nerve damage that can affect the trunk region of the body, mostly the hips, buttocks, or thighs. It can also affect the chest area. It usually affects one side of the body, but may rarely spread to the other side.
Symptoms of proximal neuropathy can include:
- Severe pain the affected regions (hips, buttocks or thighs)
- Pain over the chest or abdominal wall
- Weakness and thinning of the muscles
- Weight loss due to decrease in muscle mass
- Difficulty in standing up from sitting position (in advance stages)
When should I visit a doctor?
You should visit your doctor if you have any of the following:
- Reduced touch, pain or temperature feelings in your hands or feet
- Sharp pain, burning or tingling sensations in your limbs
- A cut or sore in the foot that is not healing
- Light-headedness or fainting spells when rising up from sitting or lying positions
- Problems in your digestion, urination or sexual activities
According to the American Diabetes Association (ADA), you should get screened for neuropathy by the doctor once you are diagnosed with Type 2 diabetes or 5-years after you have been diagnosed with Type 1 diabetes. After that you should visit your doctor for neuropathy screening at least yearly once.
References
- Pop-Busui R, Boulton AJ, Feldman EL, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017;40(1):136–154.
- Feldman, E.L., Callaghan, B.C., Pop-Busui, R. et al. Diabetic neuropathy. Nat Rev Dis Primers 5, 41 (2019).
- Deli G, Bosnyak E, Pusch G, Komoly S, Feher G. Neuroendocrinology. 2013;98(4):267-80.
- Diabetic neuropathies: diagnosis and management. Izenberg A, Perkins BA, Bril V. Diabetic neuropathies. Seminars in Neurology. 2015;35(4):424–430.
- Hicks CW, Selvin E. Epidemiology of Peripheral Neuropathy and Lower Extremity Disease in Diabetes. Curr Diab Rep. 2019 Aug 27;19(10):86.
- Retinopathy, Neuropathy, and Foot Care: Standards of Care in Diabetes- 2023. Diabetes Care 2023;46(Supplement_1):S203–S215.
